November: Diabetes Awareness Month
Submitted by Yomarie Bernier-Casillas on
Did you know that diabetes is one of the leading causes of death in the world and of which there is no cure? Diabetes is a chronic disease that affects the body's ability to use the energy contained in food. As a result, blood sugar (glucose) levels increase, resulting in a chain of short and long-term adverse effects. Depending on the type of diabetes patients need insulin or pills to control it.
After consuming food, our body transforms it into glucose and other nutrients that are absorbed by the blood. After eating, blood sugar level increases activating the pancreas that generates insulin and releases it into the bloodstream. In people with diabetes this does not happen because the body is not able to produce or react to insulin properly.
Among the various types of diabetes, type 1 has been the leading cause of death as a result of poor diagnosis. On the occasion of diabetes awareness month it is important to highlight the characteristics and symptoms of type 1 diabetes.
Most common types of diabetes:
- Type 1 diabetes: it is also known as insulin-dependent diabetes. It usually begins during childhood or adolescence but there have been cases in adulthood. It represents 5-10% of diabetes worldwide.
- Type 2 diabetes: it is the most common type of diabetes, with 95% of cases in adults. The pancreas produces insulin but the body is resistant to it. It is controlled with diet, exercise and pills. Some cases require insulin.
- Gestational Diabetes: develops during pregnancy because the body creates insulin resistance and disappears after delivery. It must be controlled since it can affect the baby due to its circulation through the placenta.
- Latent Autoimmune Diabetes of Adults (LADA): slow-progressing diabetes where there is insulin production over a long period of time. It is believed to be a subcategory of type 1 diabetes.
- Maturity Onset Diabetes of the Young (MODY): it is inherited through generations. There are different types as a result of a change in a gene. So far, 6 genes have been identified. They usually do not need insulin treatment but can be controlled with diet and pills just like type 2 diabetes.
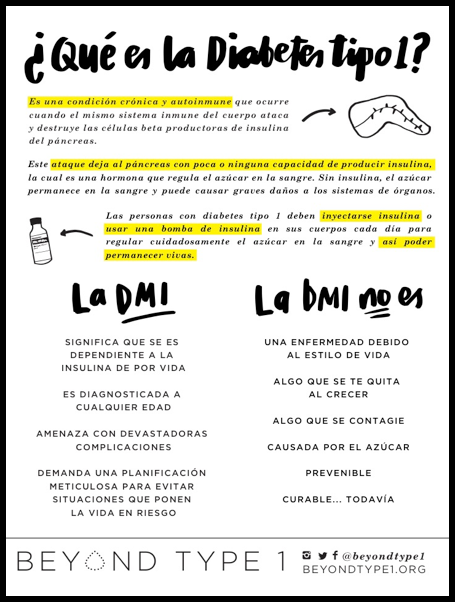
Type 1 Diabetes
It is an autoimmune disease that is characterized by selective destruction of pancreatic cells (pancreatic beta cells). Over time, high glucose levels lead to more serious complications. Its origin is unclear but it is believed that autoimmune diseases, viral infections, genetic disposition and environmental factors may play a role.
Among the main symptoms are:
- Insatiable thirst
- Increased urination
- Fatigue and increased appetite
- Unusual weight loss
- Wounds that heal slowly
- Humor changes
- Nausea or vomiting
The current problem is the late diagnosis since the symptoms are very similar to those of other conditions such as the flu. The patient enters a diabetic ketoacidosis (DKA) that can lead to death or irreversible brain damage. Ketoacidosis begins when the body use fats instead of using sugar as an energy source (due to lack of insulin). Upon decomposition (fats) ketones accumulate in the blood, which are toxic at high levels.
Treatment: consists of lifelong use of insulin, as there is no cure.
- Injectable insulin: consists of a long-lasting or basal dose and a dose of fast acting insulin with each food consumed.
- Insulin pump: this technology involves the use of rapid acting insulin. The equipment is designed to provide small doses of insulin every hour (basal) and the patient adds the amount of carbohydrates to ingest with each food to obtain the appropriate dose at the time (bolus).
- Glucometer: patients with type 1 diabetes should measure blood sugar levels with a glucometer 7-10 times a day.
- Continuous glucose monitoring (CGM): this technology consists of a sensor injected subcutaneously that allows a constant reading of blood sugar levels. The transmitter is connected directly to an insulin pump, to a receiver or to a cell phone (depending on the type of provider) emitting an alarm when the sugar levels are out of range.
- Diabetic alert dog: dogs trained to detect sugar levels by smell. These dogs can alert the patient or someone else when levels are out of range. Many of these animals have been able to alert before any technological equipment.
Short-term consequences
- Hypoglycemia: low blood sugar level (less than 70 mg / dl). There are symptoms such as weakness, tremor, sweating, irritability, and problem to think clearly, among others. If it gets too low, the patient may faint, have seizures and go into a coma. It is important to treat the symptoms by consuming carbohydrates in a controlled manner to avoid a sudden increase. If the patient is unconscious or unable to eat, then an injection of glucagon is administered, which increases the level of sugar.
- Hyperglycemia: high blood sugar level (greater than 250 mg / dl). Symptoms include: nausea, vomiting, urinating more than usual, abdominal pain, irritability, blurred vision, among others. If the levels remain elevated for a long period of time then there is a risk of producing blood ketones.
Long-term consequences
- Damage to the nerves (diabetic neuropathy)
- Erection problems
- Eye problems, including diabetic retinopathy, retinal detachment, glaucoma and cataracts.
- Diabetic foot
- Infections of the skin, female genital tract and urinary tract.
- Kidney disease (diabetic nephropathy)
- Stroke
- Diabetic angiopathy
Prevalence in Puerto Rico
- In Puerto Rico, diabetes is the third leading cause of death after heart disease and cancer.
- In the United States, about 29.1 million people suffer from diabetes, according to the American Diabetes Association. However, in Puerto Rico the prevalence is almost double (14.9%), which predominates more among women.
- Data collected by the Surveillance System show that from the total number of diabetic patients, 18% have heart conditions where 15% have suffered a heart attack and 5.8% have suffered a stroke.
- It was also reflected that 60% of adults suffer from hypertension and 8 out of 10 people with diabetes have high cholesterol.
- 43% are obese, while 36% of patients are overweight.
- In type 1 diabetes, the prevalence is 10% of the adult population, but there are only 10 endocrinologists on the island to treat them. Therefore, the treatment is extended since patients have to wait between 6 months and 1 year for an appointment.
- Approximately 200 new pediatric cases are diagnosed annually in Puerto Rico, according to data from the Pediatric Diabetes Foundation.
What can I do?
- Education: type 1 diabetes involves an insufficiency in the production of insulin, therefore the patient has no restrictions on the consumption of food (including sweets) as long as the amount of insulin needed to cover them is injected. It is always recommended a balanced diet to avoid other long-term risks but that does not mean that you cannot leave it from time to time.
- Early detection: require blood tests as part of the requirements for children and young people during a general examination when visiting the pediatrician. A blood sugar test with a glucometer or presence of glucose in urine with a strip is a simple way to detect any abnormality. Do not accept a diagnosis of a viral disease when it is possible to be diabetes. Remember that a simple drop of blood can prevent other complications.
- Do not support ads or deceptive programs: medical conditions are often used as a mocking method to attract followers. Announcements stating that the consumption of certain foods can cause diabetes are not correct; remember that children with type 1 diabetes are spectators. Learn to differentiate among the different types of diabetes.
Remember, type 1 diabetes cannot be prevented and there is no way to predict who will acquire it. Living with diabetes is a challenge because it involves changes in lifestyle, diet and physical activity. You acquire new routines, mostly, by medical procedures that can be painful or tedious. Many times those around the diabetic patient assure that the individual is not "different", however, it is. Recognizing those differences, without emphasizing them, can lead to a better emotional and social adjustment.
References
- Project Blue November - http://www.projectbluenovember.com/
- JDRF - http://www.jdrf.org/
- Asociación puertorriqueña de Diabetes - http://diabetespr.org/
- American Diabetes Association - http://www.diabetes.org/?referrer=https://www.google.com/
- Beyond Type 1 - https://beyondtype1.org/
- Centro de Diabetes de Puerto Rico - http://www2.pr.gov/agencias/diabetes/Pages/default.aspx
- El Nuevo Día – www.endi.com
- Center for Disease Control and Prevention - https://www.cdc.gov/diabetes/